Health in Transition
Trends, structural Challenges, and persistent Inequalities
The WHO describes health as physical, mental, and social well-being. This holistic definition shows that health is shaped by social, psychological, economic, and preventive influences.
Profound demographic, social, and technological changes have led to noticeable shifts in the burden of disease and healthcare systems. Only with a comprehensive understanding of these complex interrelationships can developments be anticipated and long-term financing of healthcare be secured.


Health Trends and Systemic Deficits
The high availability of information often leads to information overload and makes it difficult to identify reputable and evidence-based health sources. Interpreting medical studies or recognizing advertising for health products is particularly problematic for many laypeople.
There are deficits in nutrition education, especially among socially disadvantaged groups, partly because access to healthy food and educational opportunities for children remains limited.
Health apps and wearables promote an individualized view of health, but at the same time harbor risks of misinterpretation and medically problematic self-optimization, as medical supervision is often lacking.

Persistent Health Inequalities
Despite high levels of spending, there are marked health inequalities in Germany and throughout Europe. Numerous public health studies clearly show that socioeconomic status is closely linked to disease burden, use of preventive services, and life expectancy.
Structurally weak regions are doubly disadvantaged: not only do they lack the necessary infrastructure, but they also lack the financial resources for good medical care and, more importantly, for disease prevention.
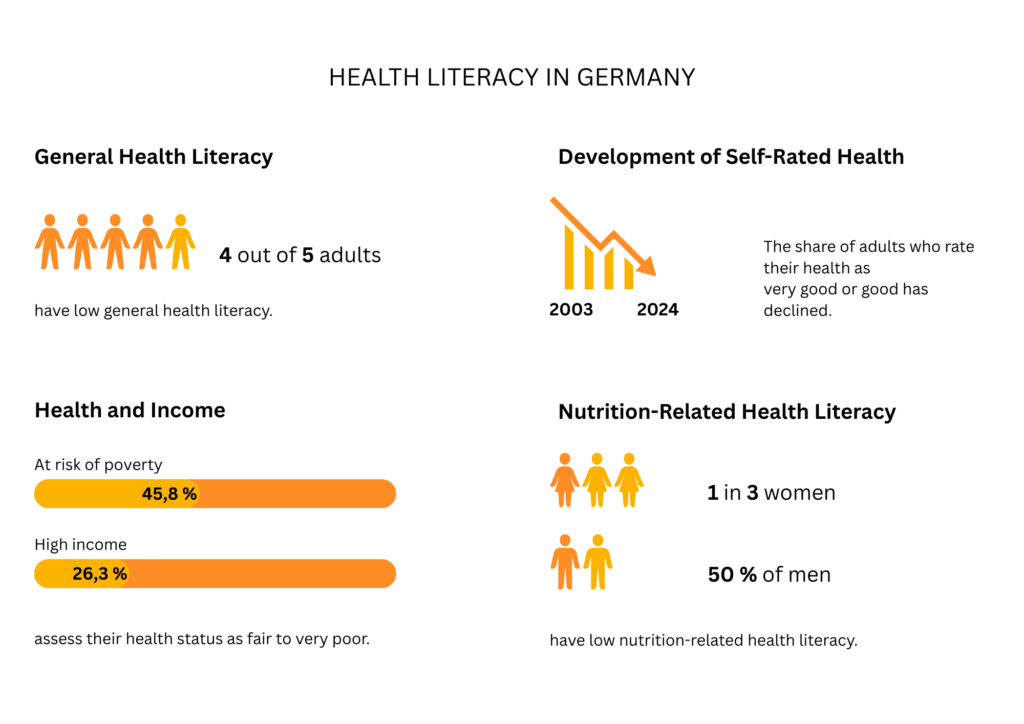
Digital solutions are not able to close these gaps and reach particularly vulnerable groups, including migrants, single parents, and the unemployed. The weaknesses of the German healthcare system are particularly evident in direct European comparison with countries such as Sweden and Switzerland, both of which achieve better results in prevention and life expectancy thanks to their centrally coordinated public health policies.
Health literacy in European comparison
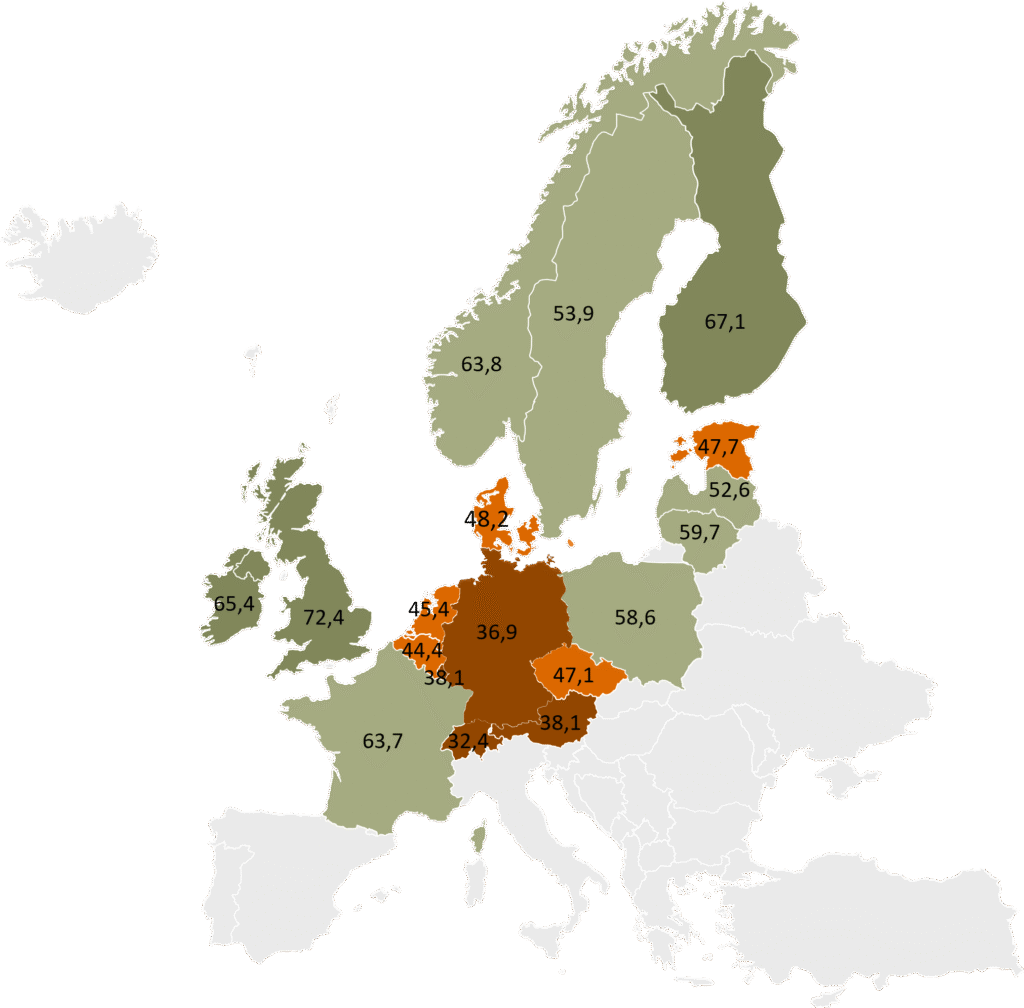
These figures reflect the effectiveness of national prevention policy—and document clear structural deficits in low-threshold services, coordination, and the teaching of health literacy.

Structural Challenges in Prevention
Prevention policy in Germany is highly fragmented and fails to reach those who need it most. Obstacles include:
- Lack of low-threshold access and relevance to everyday life
- Unregulated health communication and growing misinformation
- Regional differences that particularly disadvantage migrants, single parents, and the unemployed
- Nutrition policy measures such as mandatory food labeling or targeted promotion of healthy foods are either lacking or implemented in a way that is too industry-friendly.
Plenty of Room for Improvement – and a clear Mandate
The discrepancy between technical potential and actual structures remains significant. Promoting equal opportunities in health is a social responsibility that goes beyond individual responsibility and must counteract systemic barriers. This requires socially balanced, evidence-based, institutionally coordinated, and disinformation-resilient health promotion, in which all parties and interest groups should pull together if we want to achieve sustainably improved health care for Germany.
Many sensible measures are known but are not consistently implemented: sugar tax, food traffic lights, promotion of healthy foods, or urban planning approaches to combat heat and poor living conditions. Countries such as Austria have been demonstrating since 2019 that a structural political approach is possible.
Despite all the pessimism, however, we do not want to ignore the good news: two-thirds of the German population still rate their health as good or very good – despite a general polycrisis that is causing people distress.

Anja Führbach, Market Intelligence Senior Expert
Quellen:
- https://www.aok.de/
- https://www.rki.de/
- SVP-Research






