Digital Healthcare in Numbers
Advancements seen, but opportunities remain
Hospitals have seen progress in digitalisation since the first digital maturity assessment of German hospitals (“DigitalRadar”) in 2021. The results of the interim report of the second digital maturity assessment, which was carried out in 2024, show that hospitals improved their DigitalRadar-Score from 33.3 points in 2021 to 42.5 points in 2024, an increase of 9.1 points or 27.3 percent.[1] There is a clear correlation between hospital size and the positive development of digital maturity.
Hospitals have improved across all DigitalRadar dimensions. Similar to the first survey, they performed best in the dimension “Structures and Systems”, while “Patient Participation” showed the weakest performance. In every dimension, there are hospitals with very low levels of implementation but also hospitals with very high levels.
level of fulfillment by dimension
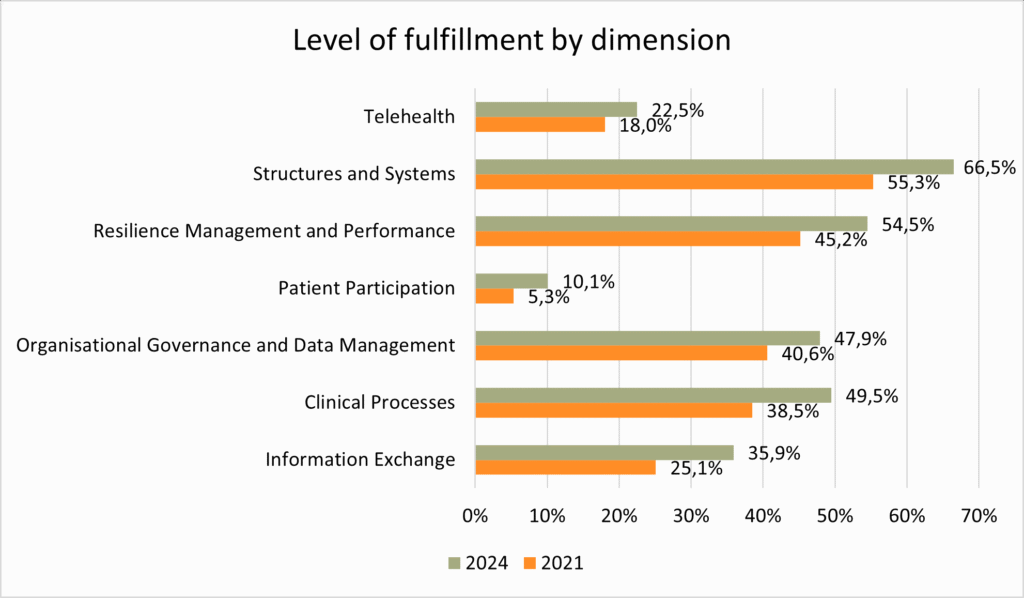
Despite the progress made since the last maturity survey, Germany still lags behind in international comparison.
[1] The DigitalRadar Score (DR Score) ranges from 0 (not digitized) to 100 (fully digitized).
Digital services offered by physician practices
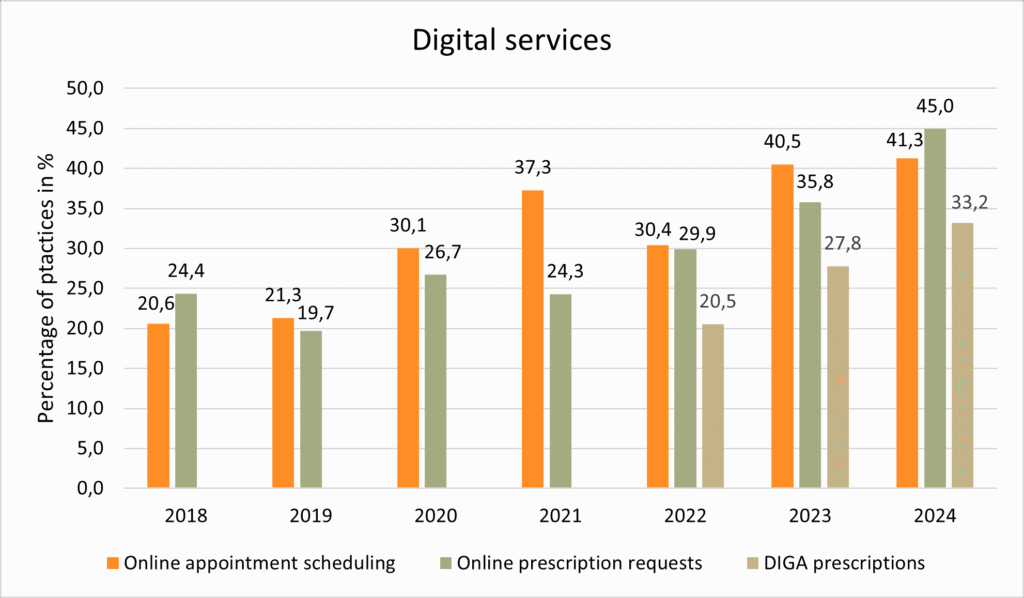
In the outpatient sector, figures from the National Association of Statutory Health Insurance Physicians (Kassenärztliche Bundesvereinigung or KBV) also indicate that practices are increasingly becoming digitalised. According to KBV surveys, there has been a significant increase in digital services offered by physician practices since 2018. This is evident in the growing use of Digital Health Apps (DiGA) online appointment booking. Electronic fit notes (eAU) and electronic prescriptions (eRezept) have also been integrated into practice routine.
As shown in the latest “PraxisBarometer Digitalisierung” (Digitalisation Barometer), the proportion of practices prescribing DiGA has been steadily increasing since 2022. Online prescription services and appointment booking are also becoming more common. The percentage of practices that offer electronic prescription rose from 24.4 percent in 2018 to 45 percent in 2024. The share of physicians offering online appointment scheduling has doubled over the same period.
digital services
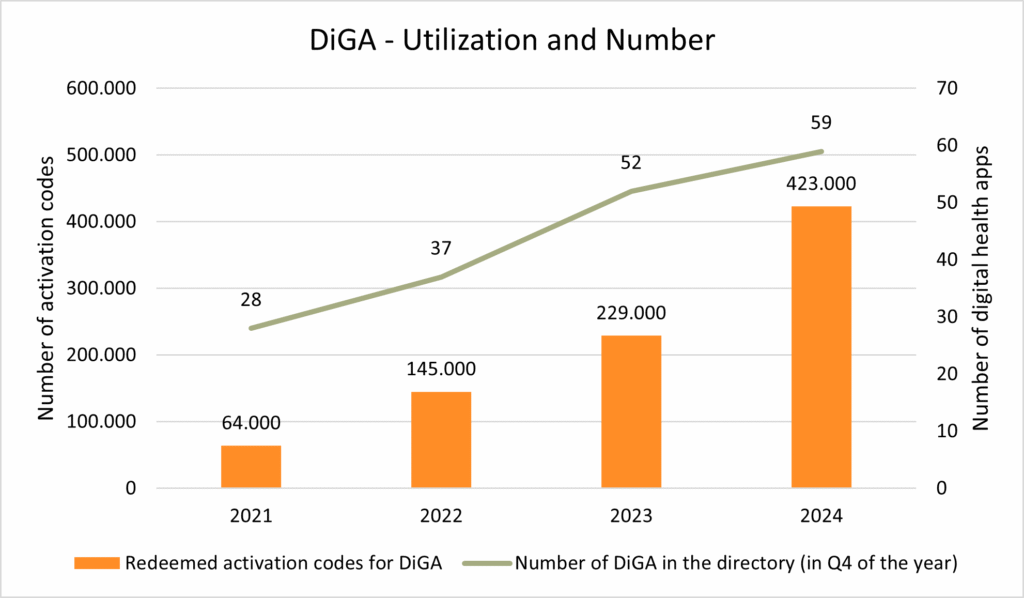
Between September 2020 and December 2024, over 1 million DiGA were prescribed by physicians or approved by Statutory Health Insurers. Of these, 861,000 DiGA were used by patients during that period. The number of redeemed activation codes continues to rise, as does the number of apps listed in the official DiGA directory.
DiGA – Utilization and Number
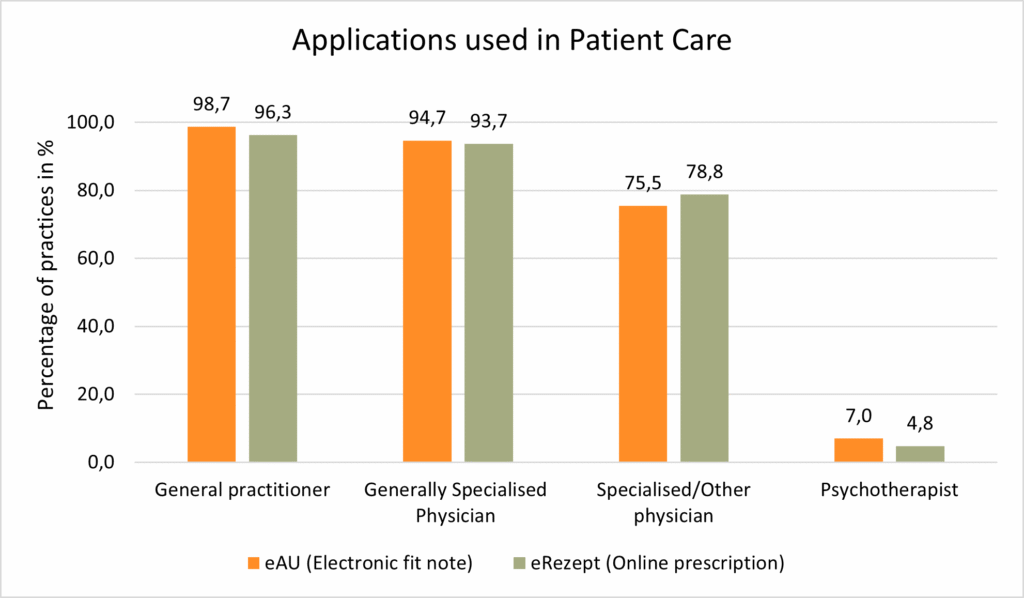
Electronic Fit notes (eAU) and online prescriptions (eRezept) have become part of the routine in practices. Across care levels, 95.1 percent surveyed practices use the eAU and 94.1 percent use the eRezept for their patients.
applications used in Patient Care
Room for Improvement: Use of the ePA and Inter-Physician Communication
The electronic patient record (ePA), on the other hand, has not yet become part of the daily routine. While it is technically installed in many practices, only a small proportion actually use it.
ePA (electronic patient record)

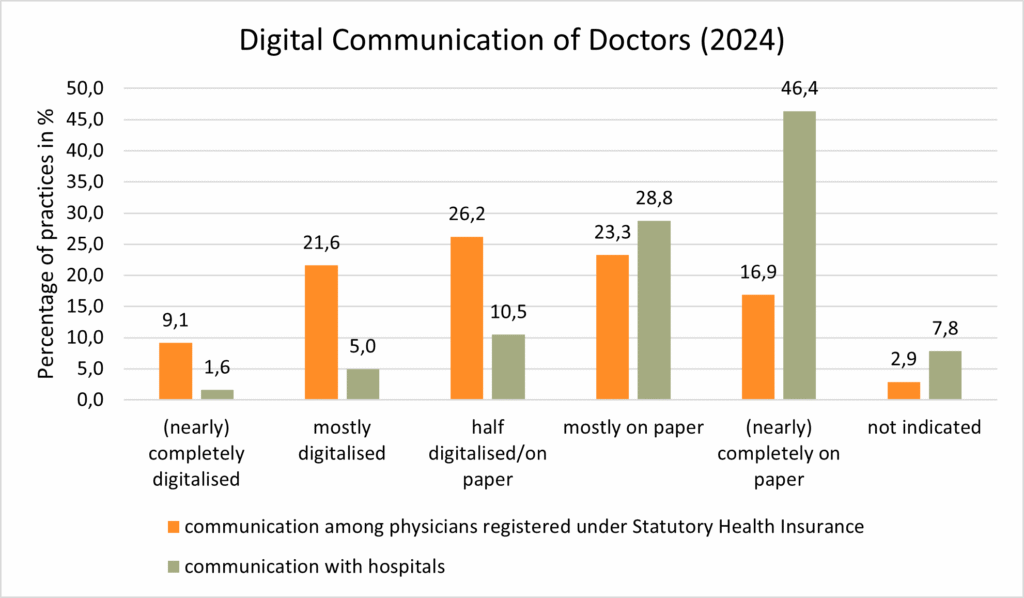
Digital communication between physicians is also not yet fully established. While physicians in practices increasingly communicate with each other via digital channels, paper is still the norm in communication between outpatient practices and hospitals.
Digital communication of doctors (2024)
Overall, both hospitals and practices are making progress in digitalisation. Nevertheless, it remains a key challenge to overcome structural, technical, and organisational barriers in order to integrate digital applications into patient care and prepare the healthcare system for the future.

Thip Pruckner, Market Intelligence Senior Expert
Sources:
- PraxisBarometer Digitalisierung 2024, IGES/KBV
- www.kbv.de
- www.aerzteblatt.de
- DigitalRadar, Ergebnisse der zweiten nationalen Reifegradmessung deutscher Krankenhäuser 2024
- Bericht des GKV-Spitzenverbandes über die Inanspruchnahme und Entwicklung der Versorgung mit Digitalen Gesundheitsanwendungen (DiGA-Bericht) gemäß § 33a Absatz 6 SGB V Berichtszeitraum: 01.09.2020–31.12.2024






